The effects of insulin on the body
Insulin is a natural hormone produced by your pancreas that controls how your body uses and stores blood sugar (glucose). It’s like a key that allows glucose to enter cells throughout your body.
Insulin is a vital part of metabolism. Without it, your body would cease to function.
When you eat, your pancreas releases insulin to help your body make energy out of glucose, a type of sugar found in carbohydrates. It also helps you store energy.
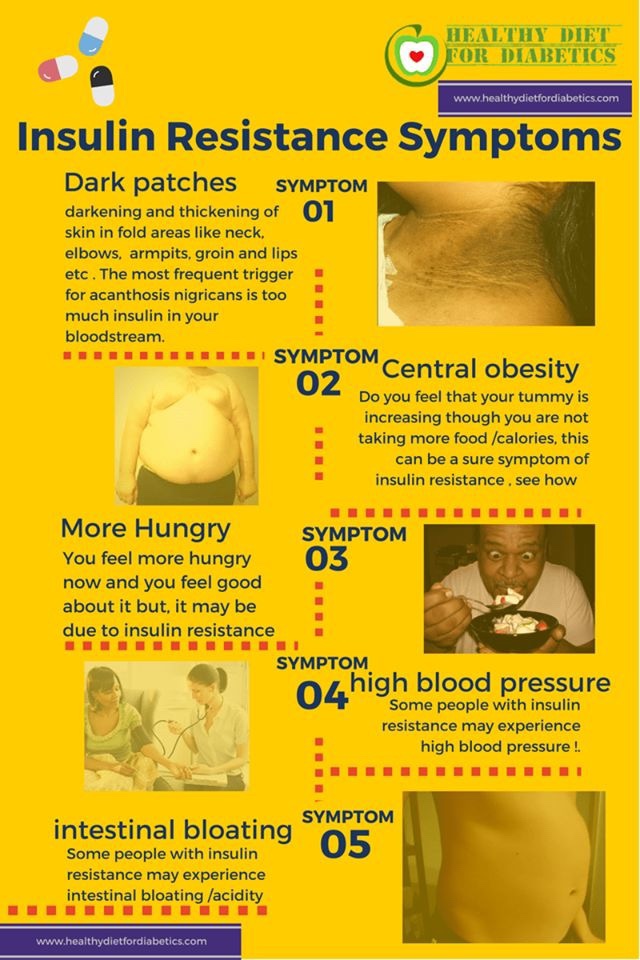
In type 1 diabetes, the pancreas is no longer able to produce insulin. In type 2 diabetes, the pancreas initially produces insulin, but the cells of your body are unable to make good use of the insulin. This is called insulin resistance.
Unmanaged diabetes allows glucose to build up in the blood rather than being distributed to cells or stored. This can wreak havoc with virtually every part of your body.
Blood tests can quickly indicate whether your glucose levels are too high or too low.
Complications of diabetes include kidney disease, nerve damage, heart problems, eye problems, and stomach problems.
People with type 1 diabetes need insulin therapy to live. Some people with type 2 diabetes must also take insulin therapy to control their blood sugar levels and avoid complications.
If you have diabetes, insulin therapy can do the job your pancreas can’t. The following types of insulin are available:
- Rapid-acting insulin reaches the bloodstream within 15 minutes and keeps working for up to 4 hours.
- Short-acting insulin enters the bloodstream within 30 minutes and works for up to 6 hours.
- Intermediate-acting insulin finds its way into your bloodstream within 2 to 4 hours and is effective for about 18 hours.
- Long-acting insulin starts working within a few hours and keeps glucose levels even for about 24 hours.
Insulin injection sites
Insulin is usually injected into the abdomen, but it can also be injected into the upper arms, thighs, or buttocks.
Injection sites should be rotated within the same general location. Frequent injections in the same spot can cause fatty deposits that make delivery of insulin more difficult.
Insulin pump
Instead of frequent injections, some people use a pump that regularly delivers small doses of insulin throughout the day.
The pump includes a small catheter that is placed in the fatty tissue underneath the skin of the abdomen. It also has a reservoir that stores the insulin and thin tubing that transports the insulin from the reservoir to the catheter.
The insulin in the reservoir needs to be refilled as necessary. To avoid an infection, the insertion site must be changed every 2 to 3 days.
Produced in the pancreas
When you eat, food travels to your stomach and small intestines, where it’s broken down into nutrients that include glucose. The nutrients are absorbed and distributed via your bloodstream.
The pancreas is a gland located behind your stomach that performs an essential role in the digestion process. It creates enzymes that break down the fat, starches, and sugar in the food. It also secretes insulin and other hormones into your bloodstream.
Insulin is created in the beta cells of the pancreas. Beta cells comprise about 75% of pancreatic hormone cells.
Other hormones produced by the pancreas are:
- glucagon, which alerts your liver to raise your blood sugar if it gets too low
- gastrin, which stimulates the production of gastric acid in your stomach
- amylin, which helps control your appetite
Energy creation and distribution
The function of insulin is to help transform glucose into energy and distribute it throughout your body, including the central nervous system and cardiovascular system.
Without insulin, cells are starved for energy and must seek an alternative source. This can lead to life threatening complications
Liver storage
Insulin helps your liver take in excess glucose from your bloodstream. If you have enough energy, the liver stores the glucose you don’t need right away so it can be used for energy later.
In turn, the liver produces less glucose on its own. This keeps your blood glucose levels in check. The liver releases small amounts of glucose into your bloodstream between meals to keep your blood sugars within that healthy range.
Muscle and fat storage
https://www.healthline.com/health/diabetes/insulin-effects-on-body
Insulin helps your muscles and fat cells store extra glucose so it doesn’t overwhelm your bloodstream.
It signals your muscle and fat tissue cells to stop breaking down glucose to help stabilize your blood sugar level.
The cells then begin creating glycogen, the stored form of glucose. Glycogen provides your body with energy when your blood sugar level drops.
When your liver can hold no more glycogen, insulin triggers your fat cells to take in glucose. It’s stored as triglycerides, a type of fat in your blood, that can be used for energy later.
Balanced blood sugars
Blood sugar, or glucose, is used by your body for energy. When you eat, it’s created by many of the carbohydrates you’re consuming. Glucose is either used right away or stored in your cells. Insulin helps keep the glucose in your blood within a normal range.
It does this by taking glucose out of your bloodstream and moving it into cells throughout your body. The cells then use the glucose for energy and store the excess in your liver, muscles, and fat tissue.
Too much or too little glucose in your blood can cause serious health problems. Besides diabetes, it can lead to heart, kidney, eye, and blood vessel problems.
Healthy cells
Cells in every part of your body need energy to function and remain healthy. Insulin provides the glucose that cells use for energy.
Without insulin, the glucose remains in your bloodstream, which can lead to dangerous complications like hyperglycemia.
Along with glucose, insulin helps amino acids enter the body’s cells, which builds muscle mass. Insulin also helps cells take in electrolytes like potassium, which keeps your bodily fluids level.
In the bloodstream
When insulin enters your bloodstream, it helps cells throughout your body — including in your central nervous system and cardiovascular system — to absorb glucose. It’s the circulatory system’s job to deliver insulin.
As long as the pancreas produces enough insulin and your body can use it properly, blood sugar levels will be kept within a healthy range.
A buildup of glucose in the blood (hyperglycemia) can cause complications like nerve damage (neuropathy), kidney damage, and eye problems. Symptoms of high blood glucose include excessive thirst and frequent urination.
Too little glucose in the blood (hypoglycemia) can make you feel irritable, tired, or confused. Low blood sugar can lead to loss of consciousness.
Ketone control
Insulin helps your cells use glucose for energy. When cells can’t use the extra glucose, they begin to burn fat for energy. This process creates a dangerous buildup of chemicals called ketones.
Your body tries to get rid of the ketones through your urine, but sometimes it can’t keep up. This can lead to a life threatening condition called diabetic ketoacidosis (DKA). Symptoms include sweet-smelling breath, dry mouth, nausea, and vomiting.HEALTHLINE CHALLENGESLooking to cut back on sugar? We’ll give you some sweet tips