As with any information, seek medical help and answers before trying something new on your own. I did not write this nor do I agree or disagree with the article. I am just passing along information so you can make a informed decision on your own.
MwsR
Metformin vs Berberine for Diabetes (Plus this yellow herb lowers blood pressure, fights parasites, and more)

By: Cat Ebeling, co-author of the best-sellers: The Fat Burning Kitchen, The Top 101 Foods that Fight Aging & The Diabetes Fix
Type 2 diabetes is fast becoming a real epidemic in civilized countries. The statistics show an ever-increasing trend of obesity, diabetes and its related complications like heart disease, kidney disease and peripheral neuropathy. Many experts are convinced that this fast-growing tidal wave of diabetes is the result of the global expansion of sugar, sugary soft drinks and major food corporations getting people addicted to terrible processed foods that are cheaper than most healthy foods and are heavily advertised to the masses.
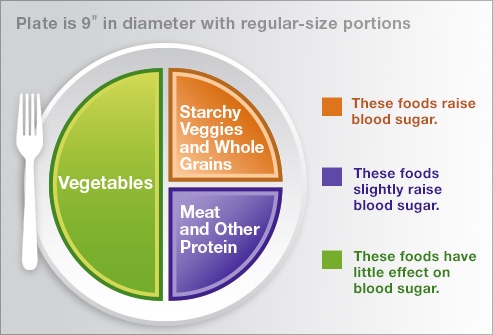
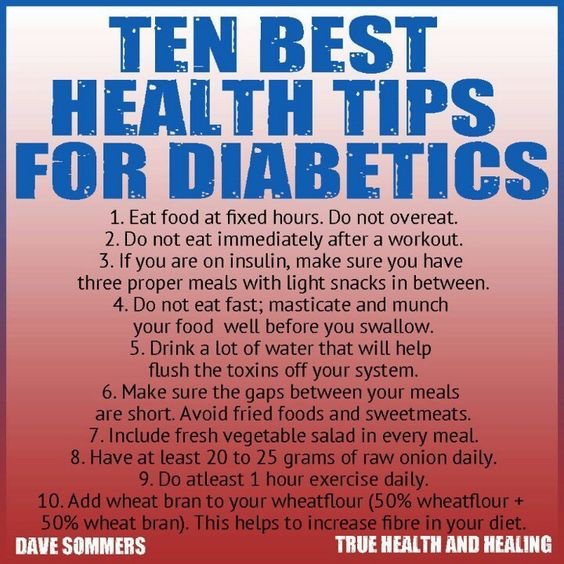
However, type 2 diabetes has the potential to be completely reversed following dietary and lifestyle changes that dramatically reduce or eliminate sugar and starches.
Relying on lowering blood sugar with medication or insulin will not improve one’s health, nor will it counteract the effects of diabetes. In fact, relying on medications to lower blood sugar actually does NOT reduce the risk of death from any of the related health complications of diabetes of stroke, heart attacks, infections, and kidney disease. Aside from the fact that diabetes drugs do not actually do anything positive for a diabetic’s health, there are many negative side effects, many of which can be downright deadly.
In one large study, called the ACCORD study, that was published in the New England Journal of Medicine in 2008, the 10,000 patients who were being treated with insulin or blood sugar-lowering drugs were monitored and evaluated for their risk of heart attack, strokes and death. The National Institutes of Health ended the study early because the medical intervention was leading to MORE deaths, heart attacks, and strokes.
Many of the conventional medical methods for lowering blood sugar actually increase insulin levels, which in turn causes more harm overall. Avandia, one of the world’s best-selling diabetes drugs, has over 50,000 lawsuits filed in the United States alone, because the drug makers failed to inform patients about possible life-threatening side-effects that include stroke, heart failure, heart attack, bone fractures, vision loss and death.
While many of these drugs do lower blood glucose levels, there seems to be no real evidence that any of the diabetes drugs actually reduce the risk of the complications of diabetes.
Most diabetes medications aim to increase insulin in the body to counteract the ever-rising levels of glucose. One of the big issues with this conventional treatment is the negative side effects that actually seem to exacerbate the complications of diabetes. Below is a list of most used diabetes meds and their primary side effects:
- Metformin — Metformin increases insulin sensitivity. Metformin also lowers glucose production in the liver. Side effects include nausea and diarrhea, and weight gain. Another significant, documented side effect of Metformin is Vitamin B12 depletion, further increasing the chances of neuropathy.
- Sulfonylureas—This class of medications help your body secrete more insulin. Side effects include low blood sugar and weight gain.
- Meglitinides – These medications stimulate the pancreas to secrete more insulin. Side effects include low blood sugar and weight gain.
- Thiazolidinediones – Like metformin, these medications make the body’s tissues more sensitive to insulin. This class of medications has been linked to weight gain and increased risk of heart failure and fractures. Rosiglitazone (Avandia) and pioglitazone (Actos) are examples of thiazolidinediones.
- SGLT2 inhibitors. They prevent the kidneys from reabsorbing sugar into the blood. Instead, the sugar is excreted in the urine. Side effects may include yeast infections, urinary tract infections, increased urination and hypotension.
- Insulin therapy. Some people need insulin therapy as well. Insulin lowers blood glucose and is a fat storing hormone, so it causes weight gain. Insulin promotes inflammation in the body when used in excess, causes hormone imbalance and increases body fat storage.

Keep in mind, however, that while most of these diabetes medications may lower blood sugar levels, increase insulin, or make the body more sensitive to insulin, they still do not prevent the serious and life-threatening complications of diabetes: High blood pressure, high LDL cholesterol, high triglycerides, poor sex drive, infertility, blood clots, kidney failure, infections and amputations, cancer, depression, heart disease, strokes, and Alzheimer’s, and more.
Insulin treatment also creates a greater susceptibility to cancer. The connection between diabetes and cancer is fairly clear—in fact, several studies have shown up to a 30% great likelihood that diabetic patients on supplemental insulin can develop colon, breast or prostate cancers.
Berberine for Type 2 Diabetes Shown to be as Effective as Diabetes Medication
There are a few natural solutions to helping to treat type 2 diabetes, and berberine is one that has a strong background of being especially effective for type 2 diabetes.
Berberine is a powerful plant extract with several impressive health benefits. It can effectively lower blood sugar, help with weight loss and improve heart health—two things that most pharmaceutical diabetic medications cannot do. It is also anti-inflammatory and antimicrobial and is effective against diarrhea, intestinal parasites, Candida albicans, and possibly Methicillin-resistant staph aureus.
Berberine works to:
- Decrease insulin resistance, making the blood sugar lowering hormone insulin more effective.
- Increase glycolysis, the breakdown of glucose inside cells.
- Decrease glucose production in the liver.
- Slow the digestion of carbohydrates.
- Increase the number of beneficial bacteria in the gut.
Berberine is a bioactive plant extract that comes from several different types of plants, including goldthread, Oregon grape root, barberry, tree turmeric and goldenseal. It has been used in both Ayruvedic and Chinese medicine for more than 2500 years and is now being used and studied extensively in the modern world.
Several impressive studies show that berberine can lower blood glucose as effectively as the drug metformin, without the negative side effects. Two of the best-known peer-reviewed studies published in the journals Metabolism and the Journal of Clinical Endocrinology compared berberine in one group to metformin (Glucophage) in another group. The berberine group had very similar blood sugar-lowering effects as the metformin group. In addition, the berberine also effectively reduced the patients’ A1C, triglycerides, LDL cholesterol, and blood pressure… Three things that metformin cannot do!
- Hemoglobin A1c decreased from 9.5% to 7.5% (about a 21% reduction)
- Fasting blood glucose (FBG) decreased from 190.8 to 124.2 mg/dl
- Postprandial blood glucose (PBG) decreased from 356.4 to 199.8 mg/dl
- Triglycerides from 100.5 to 79.2 mg/dl
Berberine works by stimulating uptake of glucose into the cells, improves insulin sensitivity, and reducing glucose production in the liver. This review published in the International Journal of Endocrinology further expanded on berberine’s role in treating type diabetes:
“BBR [berberine] is used to treat diabetic nephropathy (DPN), diabetic neuropathy (DN), and diabetic cardiomyopathy due to its antioxidant and anti-inflammatory activities.”
How does berberine work?
Berberine works by activating a metabolism-regulating enzyme within the body’s cells called AMPK (adenosine monophosphate activated protein kinase). Yes, that’s a mouthful! AMPK regulates a variety of biological activities that normalize lipid, glucose, and energy imbalances. Think of AMPK as your metabolic master switch. Definitely something you want to keep switched to ‘ON’!
Metabolic syndrome, a precursor to diabetes, occurs when these AMPK pathways are switched off. This triggers high blood sugar, high cholesterol, high triglycerides and energy issues. AMPK shifts energy to cellular repair and maintenance. Activating AMPK produces similar benefits for diabetes and metabolic syndrome as exercise, dieting and weight loss.
Berberine and Weight Loss
When overweight adults took 500mg of berberine 3 times daily for 12 weeks, they easily lost an average of 5 pounds. The researchers note that,
“…berberine has potential clinical application in reducing visceral fat and controlling obesity.”

Berberine has the ability to inhibit fat storage and also improves insulin function, leptin and adiponectin. Leptin is a very powerful hormone produced by fat cells. It tells your brain whether you should eat or not. Leptin is the way your fat cells speak to your brain. If Leptin signaling is working, when fat stores are full, they cause a surge in leptin which tells your brain to stop eating and storing fat. The problem is of course, when this signaling goes awry, it causes excessive eating and fat storage.
Adonipectin is a hormone secreted by fat cells that helps control glucose regulation and fatty acid oxidation. Obese people are often low in adonipectin, but berberine helps to increase adonipectin which helps to normalize metabolic function.
So, the bottom line here is that berberine could reduce the size of your fat cells and cut down on the number of them as well.
Berberine is also thought to enhance brown fat, which is a heat-generating special type of fat that burns energy instead of storing it. It is loaded with active mitochondria cells that convert this fat into energy which produces heat. This animal study shows how berberine increases energy expenditure, helps burn fat, improves cold tolerance and enhances active brown adipose tissue.
Berberine for Memory and Cognitive Function
Blood sugar levels, insulin sensitivity and diabetes go hand in hand with memory and cognitive dysfunction. In fact, it is now thought that high blood sugar and diabetes are connected to an increased risk of Alzheimer’s disease. Berberine has been found to enhance memory function in some animal studies, by preserving a brain chemical, acetylcholine, that is important for memory, focus and cognition. The result for berberine was improved learning and memory, along with lower oxidative stress.
How to take Berberine
According to Dr. Josh Axe, berberine should be taken two to three times a day. Generally, most studies have used safe dosages starting at 500 mg a dose. So, 500 mg two to three times a day is a good place to start. Take berberine with a meal or on a full stomach to avoid any stomach upset and to take advantage of the post meal glucose and lipid spike that often occurs. It is best to start with just one dose/day and increase slowly to ensure they can stay in control.
When you take berberine, please note that insulin may need to be cut back significantly, so monitor blood sugar frequently. Many diabetics have been able to totally stop their other pharmaceutical diabetes medications, with the inclusion of berberine. Be sure to monitor blood sugar regularly and consult your physician. Look for a berberine product with a standardized berberine extract so that the dosages and strength are consistent.
Berberine Side Effects
If you have a medical condition or are on any medications, including antibiotics, then it is highly recommended that you speak to your doctor. This is especially important if you are currently taking blood sugar-lowering medications, so that your physician can monitor your blood sugar and current medication levels.
Diabetics who are using other medications must use caution when using this supplement to avoid dangerously low blood sugar levels. People with low blood pressure should also be careful when using it since it can naturally lower blood pressure. Pregnant and nursing women should not take berberine.
Overall, this natural compound has an outstanding safety profile. Primary side effects are minor, but could result in some cramping, diarrhea, flatulence, constipation or mild stomach pain. Stay with the smaller dosages — spread out through your day and after meals — to avoid most of these side effects.
In addition to its huge benefits for diabetes, berberine is helpful for other health issues as well including:
- Anti-aging
- Gastrointestinal infections
- Heart disease
- High cholesterol
- Hypertension (high blood pressure)
- Immune challenges
- Joint problems
- Low bone density